Medical Alert IDs for Diabetes in Australia

Diabetes is Australia's fastest growing chronic condition. It is estimated that 1.8 million Australians are living with diabetes. According to Diabetes NSW & ACT, 300 people every day are diagnosed with this chronic condition. Type 2 diabetes is the most common form of diabetes in Australia. It represents 85-90% of diabetes cases each year while Type 1 diabetes represents 10-15%.
In people with diabetes, insulin is no longer produced or not produced in sufficient quantities by the body. This can lead to varying symptoms and complications which can sometimes turn into an emergency. An example of a severe complication is a diabetic coma where a person with diabetes can become unconscious. It is vital for paramedics to know that an unconscious person has diabetes. A medical ID can help to effectively communicate this medical condition and if a patient is on insulin or carries a glucagon kit to reverse severe hypoglycemia.
"Because of the risks associated with diabetes, consider wearing a medical alert bracelet indicating that you have diabetes and whether you take insulin." - Diabetes Queensland
"Wear an ID bracelet at all times, especially if you are taking insulin." - Diabetes Victoria
Hypoglycemia and Diabetic Ketoacidosis are Potentially Life-Threatening Emergencies
Studies show that an estimate 30% of diabetics experience serious hypoglycemic episodes annually. Hypoglycemia happens when a person doesn't have enough sugar or glucose in their blood. For people living with diabetes, hypoglycemia can be a result of taking too much insulin.
Signs and symptoms of low blood sugar (hypoglycemia) include:
- Feeling disoriented & confused
- Showing irritability or altered behavior
- Numbness, weakness, shaking
- Unconsciousness
The Australian Institute of Health and Welfare defines Diabetic Ketoacidosis (DKA) as a complication of diabetes that is caused by a lack of insulin. A person without enough insulin cannot use glucose for energy and instead, the body burns fat for energy. This leads to the production of high levels of blood acids, also known as ketones.
If not treated urgently, Diabetic ketoacidosis (DKA) can lead to:
- Coma
- Acute kidney failure
- Cerebral injury
- Death
"Diabetic patients should be counseled to wear a bracelet identifying their condition so EMS providers can quickly assess a diabetic emergency. Rapid identification of the emergency is needed to expedite treatment that’s necessary to prevent brain damage in hypoglycemic patients." - Journal of Emergency Medical Services
What to Engrave on a Diabetes Medical Alert ID
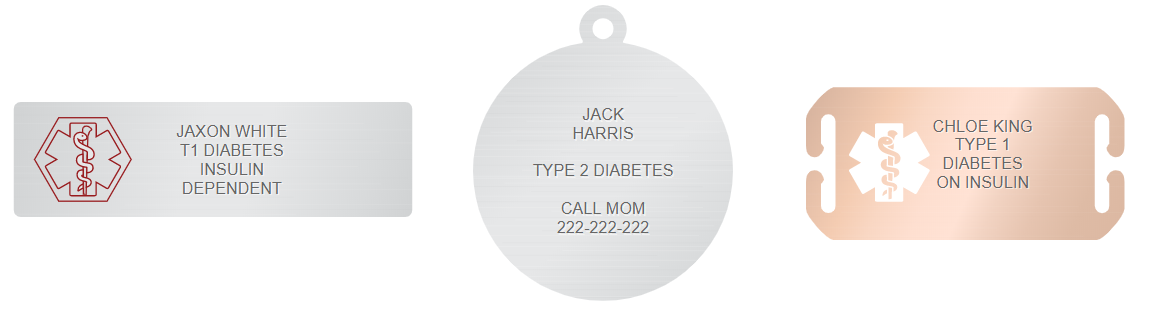
A custom-engraved medical ID is recommended to anyone who has received a diabetes diagnosis. Not all diabetes conditions are the same. Diabetes treatment plans, medications, glucose monitors, and insulin delivery devices work in different ways to manage blood sugar levels. In an emergency where every second counts, a medical alert ID should reflect a person's most accurate and up to date medical information.
The most important information to put on a diabetes medical ID are:
- Name
- Diabetes (Type 1 or Type 2) and other medical conditions
- Medications and if you carry them with you, such as an insulin pen or a glucagon kit
- Emergency contact
Common Abbreviations in Diabetes
Having sufficient space for all medical condition and emergency contact information engraving can sometimes be a challenge. These common abbreviations known to most ERs can be used as space saving alternatives:
|
AODM - Adult onset diabetes mellitus DKA - Diabetic ketoacidosis GDM - Gestational diabetes mellitus IDDM - Insulin-dependent diabetes mellitus |
NIDDM - Non-insulin dependent diabetes mellitus T1D - Type 1 diabetes T2D - Type 2 diabetes |
If you are unsure of what to engrave on your ID, a doctor can be the best source of advice on the most crucial information to include on a medical alert ID. If a lot of details need to be engraved, choose a medical alert ID tag, charm, or pendant that can be engraved on both sides. An emergency wallet card is also usually used to supplement information found on a medical ID.

The most important thing to me is that a medical ID can identify my medical condition in an emergency.
Paramedics here in Australia are trained to look for bracelets, necklaces and even tattoos.
- Frank Sita, Type 1 Writes

 - US
- US  - UK
- UK  - Canada
- Canada 